Comprehensive Chronic Liver Disease (CLD) Diagnosis & Treatment in India
Chronic Liver Disease: Chronic liver failure develops more slowly than acute liver failure. It can take months or even years before you exhibit any symptoms. Chronic liver failure is often the result of cirrhosis, which is usually caused by long-term alcohol use or viral infections like hepatitis b and c. Cirrhosis occurs when healthy liver tissue is replaced with scar tissue. During Chronic liver failure, your liver becomes inflamed. This inflammation causes the formation of scar tissue over time. As your body replaces healthy tissue with scar tissue, your liver begins to fail. The liver is the body’s largest internal organ. It lies up under your ribs on the right side of your belly. The liver does many important things including: Removes waste from the body, such as toxins and medicines Makes bile to help digest food Stores sugar that the body uses for energy Makes new proteins Common causes of Chronic Liver Failure include: Hepatitis B Hepatitis C Long-term alcohol consumption Autoimmune liver disease Non-alcoholic steatohepatitis (NASH) Hemochromatosis: inherited disorder which causes your body to absorb and store too much iron. It can build up in your liver and cause cirrhosis. What are the symptoms of Cirrhosis? Your symptoms may vary, depending on how severe your cirrhosis is. Mild cirrhosis may not cause any symptoms at all. Symptoms may include: Yellowing of the skin and eyes (jaundice) Fluid buildup in the belly (ascites) Easy bruising GI bleeding either blood in vomiting or stool Loss of appetite Weight loss Muscle loss Low energy and weakness (fatigue) Confusion as toxins build up in the blood Kidney failure How is Cirrhosis diagnosed? Your healthcare provider will take a detailed history of your past health. Then physical examination will be performed to look for signs of chronic liver disease. You may also have tests including: Blood tests: These will include liver function tests to see if the liver is working the way it should. You may also have tests to see if your blood is able to clot. Ultrasound: It uses high-frequency sound waves and a computer to create images of blood vessels, tissues, and organs. CT scan: This is an imaging test that uses a series of X-rays and a computer to make detailed images of the body. A CT scan shows details of the liver & other organs, bones, muscles, and fat. MRI: This test makes detailed pictures of organs and structures inside your body. It uses a magnetic field and pulses of radio wave energy. A dye may be shot (injected) into your vein. The dye helps the liver and other organs to be seen more clearly on the scan. Endoscopy: A lighted flexible camera is placed through your mouth into your upper digestive tract to look for enlarged blood vessels that are at risk of bleeding because of your cirrhosis. How is Cirrhosis treated? Cirrhosis is a progressive liver disease that happens over time. The damage to your liver can sometimes be reversed or improved if the trigger is gone, such as by treating a viral infection or by not drinking alcohol. The goal of treatment is to slow down the buildup of scar tissue and prevent or treat other health problems. In many cases, you may be able to delay or stop any liver damage. If you have hepatitis, it may be treated to delay the worsening of your liver disease. Eating a healthy diet which is low in sodium Avoid alcohol consumption Managing other health problems that happen because of cirrhosis Talk to your doctor before taking prescription medicines, over-the-counter medicines, or vitamins. If you have severe cirrhosis that can’t be managed medically, a liver transplant is the only option. Other treatments may be specific to your cause of cirrhosis, such as controlling excessive iron or copper levels, treating viral infection using antivirals, or using immune-suppressing medicines if it is autoimmune-related cirrhosis.
Comprehensive Acute Liver Failure (ALF) Diagnosis & Treatment in India

Acute Liver Failure (ALF): Acute liver failure occurs when your liver rapidly loses its ability to function. Acute liver failure (ALF) is a serious condition requiring intensive monitoring and urgent specialist care. If not managed properly, it’s almost always fatal. Our “Liver team” is geared to provide the required medical treatment, intensive care, and if indicated surgical care (liver transplant) for these patients. Patients with acute liver failure are treated in the liver intensive care unit (Liver ICU). Common causes of Acute Liver Failure: Hepatitis A, E, B Acetaminophen overdose (Paracetamol poisoning) Ratol poisoning Drug-induced liver failure Wilson’s disease Acute fatty liver of pregnancy Treatments ALF is a medical emergency and requires prompt medical evaluation and treatment. Patients with ALF often require admission to a liver intensive care unit and are probably best managed at the center that performs liver transplantation, which can be life-saving for such patients. Treatment includes: For low blood pressure: IV Fluids. If required medications to maintain blood pressure. For hepatic encephalopathy: Oral lactulose (a laxative) and lactulose enemas. If intracranial pressure is raised: Mannitol and other neuroprotective strategies. For infections: Antibiotics or antifungal drugs For low blood sugar: Glucose is given intravenously. For bleeding: Transfusions of fresh frozen plasma (the fluid part of the blood that contains clotting factors) and, when necessary, Packed Cell Volumes (PCV). For breathing difficulty: mechanical ventilation What are the signs and symptoms of Acute Liver Failure (ALF)? The initial symptoms of liver failure can be due to many conditions. Because of this, liver failure may be initially difficult to diagnose. Early symptoms include: Nausea Loss of appetite Fatigue Diarrhea However, as liver failure progresses, the symptoms become more serious, requiring urgent care. These symptoms include: Jaundice Weakness Excessive sleepiness Confusion Coma How to diagnose Acute Liver Failure (ALF)? Investigations to diagnose Acute Liver Failure include: Blood tests: Blood tests are done to determine the current status of the liver as well as the cause of liver failure. A prothrombin time test measures how long it takes your blood to clot. With acute liver failure, blood doesn’t clot as quickly as it should. Imaging tests: Usually, an ultrasound of the abdomen with a liver Doppler is performed to rule out chronic liver disease. Sometimes abdominal computerized tomography (CT) scan is recommended to evaluate the liver and its blood vessels. These tests can look for certain causes of acute liver failure, such as Budd-Chiari syndrome or tumors. They may be used if there is any suspicion of ultrasound. Arterial ammonia: When the liver is not working properly as in the case of acute liver failure, the blood ammonia level rises. If the blood ammonia level is very high, the patient might need dialysis support.
Pediatric Liver Transplant

Liver Transplantation for Children Your child needs a full evaluation before he/she can be placed on the transplant waiting list. The team will do many tests, including: Blood tests. Includes complete blood counts, liver function test, kidney function test, blood group, viral markers, etc. Diagnostic tests. Tests are done to check the child’s liver and general health. These tests may include X-rays, ultrasounds, and 2D echocardiography if required liver biopsy. Types of liver transplant: Living-donor liver transplants Many transplant centers throughout the world have improved the technique of living-donor liver transplantation. Current data implies that the results of living-donor liver transplant are at least similar to and possibly better than, cadaveric donor liver transplantation. The basis for taking a part of a living person’s liver lies in the organ’s capacity to grow back (regenerate) to its normal size. A part of the liver (a lobe) can be removed without causing any damage to liver function. Deceased-donor liver transplants In most cases, a healthy liver will come from a brain-dead organ donor. Either a whole liver or a part of the liver may be transplanted. While a liver transplant is the only treatment for many patients with end-stage liver disease, there are not enough cadaveric donor livers to meet the needs of all possible recipients. Split-liver transplants involve sharing a cadaveric donor’s liver so that two recipients (one small child and one adolescent or adult) may benefit from one liver donation. What is a pediatric liver transplant? A liver transplant is surgery to replace a diseased liver with a healthy liver from another person. The new liver may come from an organ donor who is brain dead or part of a liver may come from a healthy living person. This is called a living donor. A living donor should be a family member. The liver is the only organ in the body that can replace (regenerate) lost or damaged tissue. The donor’s liver will soon grow back to normal size after surgery. The part that your child receives as a new liver will also grow to normal size in a few weeks. Why might my child need a liver transplant? A liver transplant is suggested when your child’s liver doesn’t work well and they cannot survive without a liver transplant. Biliary atresia is the most common liver disease in children for which liver transplantation is required. This is an unusual disease of the liver and bile ducts that occurs in newborns. Other conditions may include: Liver cancer and other liver tumors Acute liver failure due to an autoimmune disorder, unknown causes, or an excess of medicine, such as acetaminophen Other hereditary liver disorders Conditions present at birth, such as Alagille syndrome or cholestatic diseases Viral hepatitis The development of too much iron in the body can damage organs. This is called hemochromatosis. Alpha-1 antitrypsin, an inherited disease that increases the risk of liver disease How do I get my child ready for a liver transplant? If your child’s pediatrician thinks he/she may be a good applicant for liver transplantation, they will refer your child to a transplantation center for evaluation. Your child will meet the transplantation team. Depending upon the child’s liver condition, the transplant team will decide on a cadaveric liver transplant listing or a living donor liver transplant. The transplantation team includes: Transplant surgeon Hepatologist Transplant anesthetist Pediatric transplant intensivist Transplantation nurses A social worker A psychiatrist or psychologist Dietician What happens during liver transplant surgery for a child? In cadaveric donor liver transplantation, once a liver is available for your child, you and your child will be advised to go to the hospital quickly. This can happen at any time, so you should be ready to go to the hospital at any time. At the hospital, your child will have some blood work and tests to check his/ her current status and also to rule out infection. Your child will then go into operation. The transplant may take a few hours. This will differ depending on your child’s case. After liver transplant surgery your child will be in the ICU for a few days and then will be shifted into the room. After transplant hospital stay will be 2 to 3 weeks. It depends on your child’s pre-transplant status and post-transplant recovery.
Living Donor Liver Transplant

Living Donor Liver Transplant A living-donor liver transplant is a surgical procedure in which a portion of the liver from a healthy living person is removed and implanted into someone’s belly whose liver is no longer working properly. The donor’s remaining liver regrows and returns to its normal size, volume, and capacity within a couple of months after the surgery. At the same time, the transplanted liver portion grows and restores normal liver function in the recipient. What you can expect? Before the procedure To be considered for a living-donor liver transplant, both the donor and recipient must undergo thorough health and psychological evaluation at a transplant center. The transplant team will discuss the potential benefits and risks of the procedure in detail. For example, while the procedure often may be lifesaving for the recipient, donating a portion of a liver carries some risks for the donor which is between 0.1 to 0.3%. Matching of living-donor livers with recipients is based on blood group type, organ quality, and organ size. During the procedure On the day of the transplant, surgeons will remove a portion of the donor’s liver for transplant through an incision in the abdomen. The specific part of the liver donated depends on the size of the donor’s liver, the recipient’s weight, and the needs of the recipient. Next, surgeons remove the diseased liver place the donated liver portion in the recipient’s body, and then connect the blood vessels and bile ducts to the new liver. The transplanted liver in the recipient and the portion left behind in the donor regrow rapidly, reaching normal liver volume and function within a couple of months. Why is living-donor liver transplantation desirable? Living donor liver transplantation has some advantages over deceased donor transplantation. First, there is an improved survival rate for the adult transplant recipients who received living-donor livers over deceased-donor livers. It reduces waiting list mortality as the recipient doesn’t have to wait for a long time. As a living donor liver transplant is an elective transplant, the transplant team has enough time to assess the quality of the donor’s liver.
Liver Wellness Treatment at Wockhardt Hospital
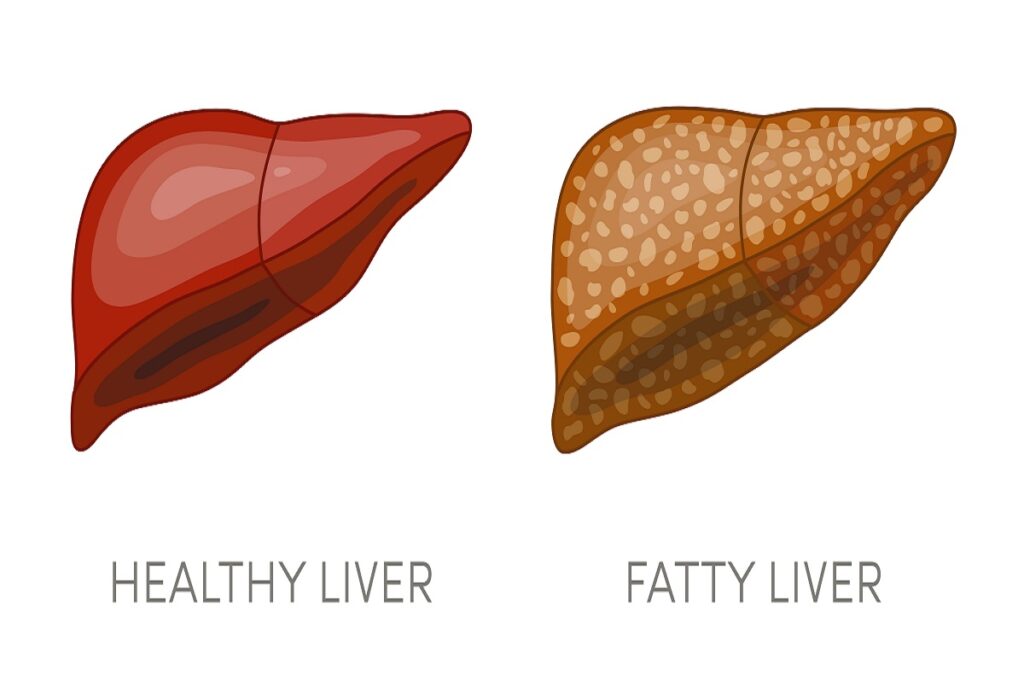
A healthy liver is crucial for the proper functioning of food digestion & detoxification. Liver diseases can be genetic or can be caused by various factors like obesity, alcohol, and viruses. Excessive alcohol or an unhealthy lifestyle can cause liver damage and lead to common liver diseases like fatty liver, hepatitis, cirrhosis, and liver cancer. Types of Liver Diseases There are various types of liver diseases & we provide complete care and treatment for all types of liver diseases. Some of the common diseases are: Cirrhosis Hepatitis (A,B,C,D,E) Liver Cancer Fatty Liver Dr. Swapnil Sharma is a liver surgeon who deals with all types of liver cancer. Liver cancers can be primary liver cancer or metastatic cancers. He also manages patients with viral hepatitis who have developed either end-stage liver disease or patients who have presented with acute liver failure. Wockhardt Hospitals Mumbai Central is recognized for its advanced infrastructure, offering a world-class environment for liver transplant procedures. The hospital boasts cutting-edge technology, including high-resolution imaging systems and a dedicated transplant ICU, ensuring exceptional patient care. The liver transplant program is backed by a highly skilled team of hepatologists, transplant surgeons, anesthesiologists, and specialized nurses, all focused on achieving the best outcomes. With a commitment to personalized care, the hospital excels in comprehensive preoperative assessments, precise surgical techniques, and effective postoperative management for long-term success
Diabetes & Stroke: Symptoms, Causes & Treatment

Diabetes is a condition that can increase the risk of developing other health conditions, particularly getting affected by a stroke, which may lead to disability and cause damage to brain tissues or even death in some cases. To prevent stroke and reduce the possibility of having a stroke, it is important for diabetic patients to understand the relationship between diabetes and stroke. Moreover, they should ensure that their blood glucose level, along with blood pressure, body weight, and cholesterol levels, are in control. More importantly, one should know the signs and symptoms of diabetic stroke to recognize it and seek medical attention immediately to prevent complications. What is a Diabetic Stroke? Diabetic stroke, or simply any stroke for that matter, is a condition in which the blood supply of the brain gets disrupted due to blockage or damage in the blood vessels supplying oxygenated blood to the brain tissue. There are two main types of stroke: Having diabetes can make it harder for the body to respond to a stroke. Diabetes can harden arteries and clog them with plaque, leading to a medical condition known as Atherosclerosis, therefore making it difficult for the arteries to deliver blood to the brain. Diabetic Stroke Symptoms Diabetic stroke has similar symptoms as that of any stroke, and it is considered a medical emergency. Therefore, it is important to look out for the following signs in a patient with diabetes. Diabetic Stroke Causes Diabetes prevents the utilization of glucose from food by the cells due to a lack of natural insulin production by the body. Diabetes also prevents insulin in the body from working to facilitate the absorption of glucose or sugar by the cells. It leads to the build-up of sugars in the body. Over time, this build-up of glucose can increase the blood sugar level, which can potentially damage the blood vessels and increase the diabetic stroke risk. Diabetic patients also suffer from a number of other health problems which can contribute to the increased risk of stroke. These health problems may include: Smoking cigarettes and alcohol consumption can pose an added diabetic stroke risk in diabetic patients. Diabetic Stroke Treatment The treatment of diabetic stroke may be done based on whether it has been identified early or has caused indelible effects. When detected early, stroke may be treated in one or more of the following ways: Long-lasting effects of stroke require rehabilitation care as stroke may impair various functions, including speech, movement, and even cognitive abilities. Preventions – How to Reduce the Diabetic Stroke Risk? If a patient has diabetes and it is suspected that their arteries have hardened up, doctors may suggest dietary & lifestyle changes along with medicines to prevent any arterial blockages that may potentially lead to a stroke. Many lifestyle changes that may help to lower the chances of diabetic stroke risk factors may include the following. Why Choose Wockhardt Hospitals? Diabetic people have a higher risk of stroke. At Wockhardt Hospitals, Mumbai, we are dedicated to managing various emergencies as well as providing comprehensive healthcare for various health conditions to prevent complications. Our doctors and medical specialists work closely with rehabilitation therapists to provide all-encompassing professional care for patients with physical and mental impairments. We are committed to providing holistic healthcare services for managing and preventing a broad spectrum of ailments and complications in our patients.
Diabetic Ketoacidosis (DKA): Symptoms, Causes & Treatment

Diabetes-related ketoacidosis, or simply Diabetic Ketoacidosis, is a life-threatening complication of diabetes in which the body does not have enough insulin to utilize glucose for energy production in the body. It turns to fats for breaking down into energy, releasing ketones in the process. These ketones turn the blood acidic, leading to a life-threatening condition. What is Diabetes-related Ketoacidosis (DKA)? Diabetic ketoacidosis is a serious and life-threatening complication of diabetes affecting those with unregulated diabetes or those who have not been diagnosed with diabetes yet. People with this condition are not able to produce enough insulin. Insulin plays an essential role in utilizing sugar or glucose for producing energy to be used by the body by facilitating the movement of sugar into the cells of the body. The insulin hormone is produced by the pancreas normally or injected into the bloodstream in diabetic patients. When there is a lack of insulin, the body may start breaking down fat to produce energy as the cells cannot utilize glucose present in the body. When the body starts breaking down fat, ketones are released into the bloodstream. When ketones start building up in the body, a high level of ketone can make the blood acidic. If left untreated or undiagnosed, it can turn into a dangerous condition known as diabetic ketoacidosis, which can give many warning signs and symptoms. This condition requires medical attention as soon as possible as it is potentially life-threatening. People with type-1 or type-2 diabetes can potentially develop diabetic ketoacidosis at any point in their lives. Therefore, it is important to stay vigilant of the symptoms exhibited by the body, and any concerning changes should be reported to a doctor to avoid complications. Diabetic Ketoacidosis Symptoms Incidentally, the symptoms of diabetes-related ketoacidosis (DKA) can appear as early as 24 hours after the body has started breaking down fat and releasing ketones into the bloodstream. For some people, these symptoms may even be the first signs of diabetes, which would then warrant a visit to the doctor to confirm or rule out the possibility. However, none of these symptoms should be ignored, especially if there is a family history of diabetes or the patient is obese and has risk factors for diabetes. The early diabetic ketoacidosis symptoms may include the following. If the condition has progressed, severe diabetic ketoacidosis symptoms may appear, which may include: Diabetic Ketoacidosis Causes The main cause of experiencing diabetes-related ketoacidosis is a lack of enough insulin in the body. The following conditions may lead to this medical condition. Diabetic Ketoacidosis Diagnosis Primary diabetic ketoacidosis diagnosis can be done by a physical examination and performing certain blood tests. The blood tests performed for diagnosing diabetic ketoacidosis may include the following. Quantitative analysis of ketone can also be done by a urine test. Other diagnostic tests used for the diabetic ketoacidosis diagnosis may include: Diabetic Ketoacidosis Treatment Diabetic ketoacidosis treatment may be treated as an emergency if the symptoms are severe. The treatments used for diabetic ketoacidosis may include the following. Fluids Frequently urinating can cause loss of fluid, thinning out blood sugar in the process. Fluids can be replenished orally or intravenously through an IV line. Electrolyte Replacement Having too little insulin in the body can also lead to the lowering of various electrolyte levels in the blood, such as sodium, potassium, and chloride. Electrolytes also need to be replaced during diabetic ketoacidosis treatment. Insulin Therapy In addition to electrolyte and fluid replacement, insulin is also administered, usually intravenously, to reverse the diabetic ketoacidosis condition. Insulin therapy may be administered until the blood sugar level becomes lower than 200 mg/dL and the blood is no longer acidic. At Wockhardt Hospitals, Mumbai, we are committed to providing exceptional diabetes treatment for a wide range of health conditions, including Diabetic Ketoacidosis, making sure all our patient’s medical needs and emergencies are well taken care of with utmost expertise and compassion. We have years of experience with all the world-class facilities and state-of-the-art infrastructure for optimal healthcare services in one place.
Diabetic Nephropathy: Symptoms, Causes & Treatment

Diabetes is a prevalent chronic condition that impacts millions of individuals worldwide. It is known to have a number of possible consequences. One of the most serious and often overlooked complications is diabetic nephropathy, a condition that affects the kidneys. While diabetic nephropathy seldom occurs in the first ten years after diagnosis in individuals with Type 1 diabetes, kidney damage can already be present in certain Type 2 diabetics at the time of diagnosis. Understanding Diabetic Nephropathy Diabetic nephropathy, or diabetic kidney disease, is a long-term complication of diabetes that primarily affects the kidneys. This medical condition arises when diabetes damages the small blood vessels and functional units within the kidneys, reducing their ability to optimally filter waste and excess fluids from the blood. Over time, this can lead to kidney dysfunction and, in severe cases, End-Stage Renal Disease, requiring dialysis or a kidney transplantation for survival. Diabetic Nephropathy Symptoms Diabetic nephropathy often develops silently, progressing without noticeable symptoms in its early stages. However, as the condition advances, the following diabetic nephropathy symptoms may become apparent: Diabetic Nephropathy Causes The primary cause of diabetic nephropathy is diabetes itself, particularly when blood glucose levels are not well controlled. There are around one million nephrons in each of our kidneys. Nephrons are tiny organelles that remove waste from the blood. Nephrons can become thicker and scarred as a result of diabetes, which reduces their capacity to filter waste and eliminate fluid from the body. They start to leak albumin, a kind of protein, into their urine as a result. High blood pressure and blood sugar are suspected to be contributing factors to diabetic nephropathy causes, while the precise cause of this condition in diabetics is uncertain. Two factors that can harm the kidneys and impair their ability to filter waste and eliminate water from the body are persistently high blood pressure and blood sugar. Risk Factors of Diabetic Nephropathy While diabetes is the major risk factor for diabetic nephropathy, certain factors can increase the likelihood of developing this condition: Diabetic Nephropathy Diagnosis Early detection of diabetic nephropathy is crucial for effective management. Several diagnostic tests and assessments can help in identifying this condition: Diabetic Nephropathy Treatment Diabetic nephropathy is a serious medical complication of diabetes that affects the kidneys and can lead to end-stage renal disease if left untreated. Diabetic nephropathy treatment involves a multifaceted approach aimed at preserving kidney function and reducing the risk of complications. The diabetic treatment plan may include the following components: Advanced Diabetic Nephropathy Treatment When kidney disease reaches an advanced stage and eventually results in renal failure, the patient’s doctor will provide targeted therapy to manage kidney function, including: Why Choose Wockhardt Hospitals? Our leading healthcare institution – Wockhardt Hospitals – is well-known for its dedication to qualitative and patient-centered treatment. With its state-of-the-art diagnostic and therapeutic facilities, the hospital guarantees that its patients get the best possible care. In order to improve their overall experience, patients at Wockhardt Hospitals may anticipate personalized treatment concerning their particular medical requirements and preferences. FAQs Q. Is the patient’s quality of life improved by dialysis? Yes, dialysis can prolong and improve a person’s life, but this will depend on their health and how well they adhere to their treatment plan. Q. When is the best time to see a nephrologist? Get checked for kidney disease every year with basic blood and urine tests if you have diabetes, high blood pressure (BP), or are over 50 years of age. The earliest signs of kidney illness are facial puffiness, limb edema, decreased appetite, and frothy urine. Q. Can nephropathy caused by diabetes be prevented? By closely monitoring diabetes and associated symptoms, including blood pressure medicine, diabetic nephropathy can be prevented or delayed in its course.
Diabetic Charcot Foot: Symptoms, Causes & Treatment

Diabetes is a health condition involving elevated levels of glucose (sugar) in the blood. It is a common health condition that affects quite a large portion of the population. Diabetic Charcot Foot is a common side effect of unregulated diabetes, and it can cause much damage if left untreated, which may not cause painful symptoms in the beginning. It requires regular screening and prompt Charcot Foot treatment to prevent damage caused by this medical condition. What is Diabetic Charcot Foot? Charcot Foot is a rare complication of diabetes-related neuropathy, which entails nerve damage that may cause loss of sensation in the lower legs and feet. This makes it impossible for the affected diabetic patient to feel pain or experience other symptoms that may be indicative of a hurting foot. Diabetic Charcot Foot may occur as a result of a small injury or infection that may cause severe complications so that they don’t feel or notice any painful symptoms. If the Charcot Foot is not treated as soon as possible, it may lead to the collapsing of joints in the affected foot, which can permanently alter the ability to unlock the full movement of the foot. It can also cause an infection in the feet to spread or worsen quickly. In severe cases, it may also lead to life-threatening conditions, which may then require amputation. The best way to prevent diabetic Charcot Foot is to keep diabetes under control and check the blood sugar level regularly. It would also be a good idea to get the feet checked regularly by a healthcare provider to look for any changes in sensation like pain, pressure, or touch. Diabetic Charcot Foot Symptoms Although it may be possible that diabetic patients with the Charcot Foot don’t feel pain initially, they may experience other symptoms. The earliest diabetic Charcot Foot symptoms may be swelling of the affected foot, which can occur spontaneously without any infection or injury. The other diabetic Charcot Foot symptoms may include: It is important to visit a healthcare provider when these symptoms appear to prevent further complications. An advanced stage of diabetic Charcot Foot may cause symptoms such as: Diabetic Charcot Foot Causes Charcot Foot is often associated with diabetic patients. It may happen when a foot gets injured or is affected by an infection. In most cases, patients with diabetic Charcot Foot do not feel pain. Sometimes, there is no specific cause for Charcot Foot, and it may be triggered by conditions like: Other medical conditions in diabetic patients that may also be diabetic Charcot Foot causes include the following: Risk Factors of Diabetic Charcot Foot Charcot Foot is almost always a side effect of unregulated diabetes or hyperglycemia (a condition of high blood sugar), leading to diabetes-related neuropathy. People who have had diabetes for more than seven years and smoke and/or drink are at a higher risk of neuropathy. A diabetic person is also likely to experience neuropathy due to other health conditions such as: Complications of Charcot Foot Unregulated high blood sugar leading to Charcot Foot may cause various complications if left untreated; these may include: Diabetic Charcot Foot Diagnosis If an individual experiences swelling, pain, or warmth in one foot, it would be best for them to visit a healthcare provider. They may provide a diagnosis based on physical examination and some imaging tests. They may examine both the feet and ankles to look for changes or differences in the feet. They may also check the degree of sensation or feelings of touch in the feet, ankles, and toes. The diagnostic tests that may be recommended by the healthcare provider or doctors may include the following: Diabetic Charcot Foot Treatment Based on the diagnosis by the healthcare provider, patients may be treated according to the symptoms and severity of the condition. As a first step towards Charcot Foot treatment, preventing further spread of the infection is necessary, for which the healthcare provider may recommend refraining from walking on the feet to worsen the condition. They may also recommend pain-relieving medications to provide relief from symptoms and reduce the impact that Charcot Foot may have on the patient’s ability to use the foot. The most common diabetic Charcot Foot treatment may include the following. Preventing Pressure on the Foot Doctors may recommend putting less pressure or weight on the feet to prevent swelling and injuries such as bone fractures from worsening. They may suggest using a supportive cane or crutch. Changes in Footwear Doctors might suggest wearing special footwear that supports the feet and keeps the toes in the right position. Such shoes may need to be custom-made, which may help relieve pressure from the ankles and feet when walking. Physical Therapy Physical therapy is a necessary Charcot Foot treatment approach to improve circulation and movements of the joints, ankles, and legs. This can help to manage symptoms such as pain and stiffness. Physiotherapy specialists may also help customize a set of exercises and movements to help patients make specific movement advances. Charcot Foot Surgery If the condition worsens, the patient may experience severe symptoms involving collapsed bones & joints, ulcers, or an infection that may have spread. Progressing of Charcot Foot may damage the foot and ankle joints. Surgery for Charcot Foot may help to repair damage and stabilize the foot. In case of advanced or severe cases, amputation of the affected area may be needed. Preventing Charcot Foot The best way to manage diabetic Charcot Foot is to prevent it by managing diabetes as well as the overall health. Controlling high blood sugar may prevent hyperglycemia and reduce the risk of neuropathy. It is also essential to get the feet checked by healthcare providers regularly to ensure optimal feet condition. A diabetic person may also reduce the risk of Charcot Foot by doing the following things: At Wockhardt Hospitals, general physicians and primary care doctors provide comprehensive healthcare services with immense care and compassion to help treat and manage a wide range of health conditions and
Diabetic Macular Edema (DME): Symptoms, Causes & Treatment

Diabetic Macular Edema (DME) is a serious eye condition that can develop in people with diabetes. This condition affects the macula, the part of the retina in charge of the near-term detailed vision, which gives it its characteristic appearance. The macula allows us to see fine details, read, recognize faces, and perform other tasks that require sharp and precise vision. A fluid leak from adjacent blood vessels causes the macula to enlarge, impairing vision and changing the appearance of colors, making them bland or faded. Diabetic macular edema symptoms can range in severity from a slight blurriness of vision to a significant loss of central vision that makes everyday tasks challenging. When DME occurs, it can lead to vision impairment or even blindness if left untreated. Diabetic Macular Edema Symptoms Diabetic Macular Edema (DME) often presents with a variety of symptoms, which can range from mild to severe. Some common diabetic macular edema symptoms include: Diabetic Macular Edema Causes Diabetic Macular Edema (DME) primarily results from complications of diabetes, particularly when blood sugar levels are poorly controlled over an extended period. Several other diabetic macular edema causes are: Risk Factors of Diabetic Macular Edema (DME) Certain factors increase the risk of developing diabetes macular edema, and understanding these risk factors can help individuals with diabetes take proactive steps to manage their eye health. Some of the key risk factors for DME include: Diabetic Macular Edema Treatment Diabetic Macular Edema treatment is essential to prevent vision loss and improve overall quality of life. Several treatment options are available, and the choice of treatment depends on the severity of the condition, the patient’s overall health, and other individual factors. The diabetic macular edema treatment includes: Wockhardt Hospitals: A Trusted Choice for DME Management Diabetes patients may develop diabetic macular edema (DME), a disease that might seriously impair their eyesight. Wockhardt Hospitals distinguishes itself as a respected healthcare establishment with the experience, technology, and patient-centered approach to efficiently manage Diabetic Macular Edema. Our world-class medical professionals offer comprehensive care, including regular eye check-ups, early detection, and a range of treatment options to meet each patient’s individual needs. FAQs on Diabetic Macular Edema (DME) Q. Is DME a serious condition? Yes, it can become a serious medical problem if treatment is not received within time. The primary cause of permanent blindness is diabetic eye disorders, which include Diabetic Macular Edema. The good news is that, with effective treatment, your vision can be preserved—especially if caught early. Q. Can I drive if I have diabetes macular edema? It is determined by the total clarity of your vision. Your doctor is the best person to help you make this decision, but when possible, it might be wiser (and safer) to find alternative transportation options. Q. Can diabetic macular edema ever be cured? There’s no treatment for DME as of yet. Nonetheless, prompt medical attention and effective diabetes treatment control may minimize blindness, prevent its advancement, and sometimes even reverse the damage.